Deep Vein Thrombosis: Causes, Symptoms, Treatment
Vein Thrombosis, commonly referred to as blood clotting, functions as a natural defense mechanism to prevent excessive bleeding following bodily injuries. Nonetheless, complications ensue when these clots form within veins, obstructing normal blood circulation. This occurrence can result in superficial thrombosis or, more critically, deep vein thrombosis (DVT). Despite DVT lacking a definitive cure, there are effective management and treatment approaches available.
What is Deep Vein Thrombosis?
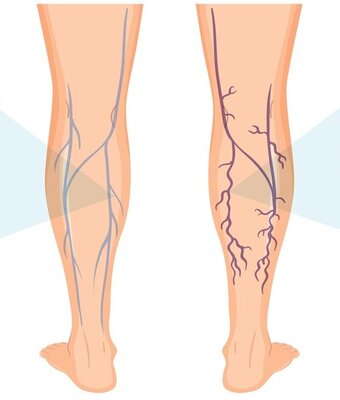
Deep vein thrombosis occurs when a blood clot (thrombus) forms in a deep vein, typically one of the large trunk veins within the muscles or bones, connecting the heart and lungs with superficial veins throughout the body. The implications of such clots vary depending on their location, with thrombosis manifesting as either an isolated incident or a chronic issue. Fortunately, proactive measures can mitigate risk factors and address the condition.
Causes of Deep Vein Thrombosis:
Several factors contribute to the likelihood of developing DVT, echoing those associated with other vein-related disorders:
- Age
- Injury to an artery, vein, or surrounding tissue
- Surgical procedures
- Prolonged periods of immobility, such as extended sitting or lying down, as experienced during long flights, car rides, hospital stays, or limb immobilization
- Genetic predisposition, especially with a family history of DVT, pulmonary embolism, or blood-clotting disorders
- Pregnancy, particularly in later stages and postpartum, necessitating increased mobility and the use of compression stockings
- Certain medications like oral contraceptives and hormone replacement therapy, which may heighten clotting risk
- Obesity, which exerts added pressure on lower limb veins
- Smoking, amplifying the risk of DVT and various other health complications
While the correlation between varicose veins and DVT remains debatable, research suggests a potential association. A study in the German journal VASA indicated that individuals with varicose veins exhibited a higher incidence of DVT, particularly when coupled with a history of venous thromboembolism or recent hospital discharge.
Symptoms of DVT
Recognizing the signs of DVT is crucial for prompt intervention. Symptoms may include:
- Persistent cramping soreness in the leg
- Throbbing or cramp-like sensations
- Pain and tenderness exacerbated by standing or walking
- Swelling and discoloration in the affected area
- Localized warmth
- Impaired mobility, with increased pain upon movement
In severe cases, a dislodged deep vein clot can travel to the heart or lungs, precipitating pulmonary embolism. Associated symptoms include:
- Shortness of breath, particularly following exertion
- Coughing up bloody or pink-tinged mucus
- Fever, excessive sweating, or clammy skin
- Lightheadedness, dizziness, or fainting spells
- Rapid or irregular heartbeat
- Intensifying chest pain exacerbated by movement or respiration
- Immediate medical attention is imperative upon experiencing any of these symptoms to prevent life-threatening complications.
Risk and Treatment of Thrombosis
The primary risk of thrombosis lies in clot dislodgment, potentially leading to pulmonary embolism. Additionally, DVT may culminate in Postphlebitic Syndrome, characterized by long-term leg swelling, pain, skin discoloration, and ulceration.
While DVT incidence is relatively low, vigilance is essential. Treatment focuses on mitigating risk factors and managing symptoms rather than curing the condition outright. Anti-coagulants, commonly known as blood thinners, and compression stockings are cornerstone interventions, supplemented by exercise and physiotherapy to enhance circulation and alleviate discomfort.
To ascertain individual DVT risk, consultation with healthcare professionals is indispensable. Diagnostic methods such as Duplex ultrasound or venography facilitate accurate assessment, guiding personalized interventions. Furthermore, lifestyle modifications and dietary adjustments can effectively mitigate hereditary or situational predispositions toward DVT.
In conclusion, while DVT presents significant health concerns, proactive management strategies empower individuals to safeguard against potential complications. Our dermatologists and vein specialists stand ready to provide expert guidance and support, ensuring optimal vascular health and well-being.
FAQ
Is deep vein thrombosis (DVT) hereditary?
While genetics can play a role, other factors like lifestyle and medical history also contribute to DVT risk.
Can DVT occur without noticeable symptoms?
Yes, it’s possible for DVT to develop silently without overt symptoms, making regular screenings important.
Are there specific dietary recommendations to prevent DVT?
Maintaining a balanced diet rich in fruits, vegetables, and lean proteins can support overall vascular health, but specific dietary strategies for preventing DVT remain inconclusive.
What should I do if I suspect I have DVT during pregnancy?
It’s crucial to seek immediate medical attention, as pregnancy increases DVT risk. Your healthcare provider can offer tailored guidance and interventions.
Are there alternative therapies or home remedies for managing DVT?
While lifestyle modifications like regular exercise and elevation of affected limbs may help, they should complement, not replace, conventional medical treatments. Always consult a healthcare professional for personalized advice.


